Prescription Claim Form

Who is eligible
Member, and eligible dependents as defined by the Fund.
What is the Benefit

The Department of Veterans Affairs (VA) charges a copayment for each 30-day or less supply of medication provided on an outpatient basis for the treatment of a non-service connected condition. The copayment amounts are. All prescription medications received through VA between April 6, 2020, and September 30, 2021 Learn more about what this means for your copayments Effective January 1, 2021 Note: Some Veterans don't have to pay copays (they're 'exempt') due to their disability rating, income level, or special eligibility factors. Our Open Funds are now accepting applications for assistance from new and renewal patients. Our Closed Funds are currently closed to new and renewal applications due to lack of sufficient funding. CPR allocates funding to all patient’s that are approved for a grant so that it is available when needed by the patient. You need to pay your full VA copay bill balance by the due date on your billing statement to avoid late charges, interest, or collection actions. Find out how to make a payment—and what to do if you're having trouble making payments or you disagree with your bill. Copay cards for patients. HCP for physicians. TERMS AND CONDITIONS. Dexcom is partnering with a pharmacy claims administrator, ConnectiveRx, to offer a limited-time trial program for patients in select areas who fill their G6 prescriptions at participating pharmacies and who either (1) have commercial health insurance coverage for Dexcom G6 CGM products but desire financial support with their.
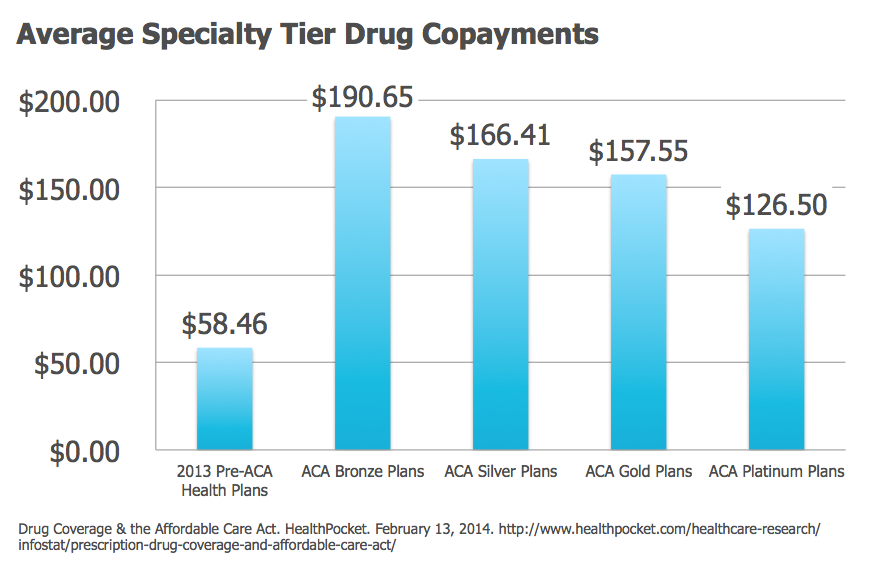
How Much Is My Copay
Once annually the Fund reimburses to a member the out-of-pocket costs that have been paid within the calendar year for drugs prescribed by a medical doctor, osteopath or dentist. Prescriptions must be dispensed by a licensed pharmacist. Please contact the Fund for the yearly maximum amount or the allowable copayment amount. All rules and regulations governing Suffolk County’s primary prescription plan apply to your Fund coverage.
Covered expenses
- Prescriptions that require compounding;
- Prescriptions for legend drugs (drugs that cannot be dispensed by a pharmacist without a prescription);
- All other drugs covered by the plan in accordance with the terms and conditions set forth by the plan.
Exclusions
- OTC (over the counter) drugs, vitamins, diet supplements, etc., which even if prescribed by a physician can be legally purchased without a prescription.
- Drugs covered by this plan must be prescribed by a licensed medical doctor, osteopathic physician or dentist
- All drugs must be dispensed by a registered pharmacy.
- Drugs which are administered to in-patients of any hospital are not eligible.
- Single prescriptions that exceed a 3-month supply (this does apply to refills obtained at a later date).
- Growth stimulating drugs, food supplements, cosmetic drugs, or any other drug prescribed for conditions other than injury, illness or disease are not covered by the plan.
- Expenses not submitted prior to December 31st of the current year for the previous year will not be eligible for reimbursement. Example: Claims for 2020 may be claimed only up to 12/31/2021
Note: The Fund will not pay prescription costs incurred by members in excess of the co-payment maximum. If you use a pharmacy that does not participate with your primary prescription carrier, you will be required to pay the full cost of the prescription to the pharmacy. To receive your benefit, submit a completed reimbursement form to your medical plan. The Fund will only pay the co-payment amount that the plan would have paid if you used a participating pharmacy.
Limitations
- Duplicate claims cannot be honored.
- Prescriptions for allergies dispensed at a laboratory will be allowed only if the prescriptions would normally be filled at a licensed pharmacy.
- Claims for prescription drug co-payments can only be filed ONCE annually per family. Submit only after you have accumulated the annual maximum for co-payment costs. If you do not meet the maximum total prior to the end of the year, submit your claim for whatever the amount is below that figure after the last day of that calendar year. Any claim paid by the Fund will NOT be reconsidered at a later date, even if you discover that you failed to include several co-pays on your original claim. Make sure that you have acquired all of the necessary pharmacy print-outs and primary prescription statements before making claim to the Fund. It is your responsibility to ensure that your original claim contains all of your families’ co-payments.
Claiming
Obtain a Prescription Drug claim form from your payroll representative or the Fund. Complete instructions for filing are included on the back of the claim form. Proof of payment must be attached.
Pharmacy Printout Filings
Complete the claim form for all persons covered under the insured’s benefit. Prescriptions for the member, spouse, and covered children must be on the same form. Identify each family member and list all printouts for that person, including the total of each one. Do this for each individual you are submitting for. Please complete all required areas of information.

Remember to sign and date the bottom of the form.
Individual Receipts
We do not accept individual receipts.
Costs
Find your TRICARE costs, including copayments,enrollment fees, and payment options.
- Most costs are for calendar year 2021 unless noted separately.
- For US Family Health Plan and TRICARE Prime Remote costs, choose 'TRICARE Prime' from the pull-down menu
- Visit the Cost Terms page for definitions to help you better understand TRICARE costs.
- If you're an unremarried former spouse, for the Continued Health Care Benefit Program (CHCBP), chose 'Retired' regardless of your sponsor's status
- Looking for dental costs? Visit the TRICARE Dental Costs section.
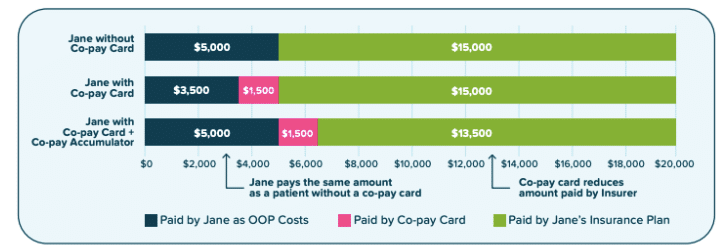
Prescription Copay Card
Copayments will be waived retroactively to March 18 for certain testing and office visits related to the testing. The test must be one approved, cleared, or authorized by the Food and Drug Administration to detect SARS-CoV-2 or diagnose COVID-19. If you paid any copayments for testing related to COVID-19 and the resulting office visits with a network or non- network provider, you may file a claim for reimbursement. For more information related to the coronavirus, visit the FAQ page.
